Time-lapse significantly improves live birth rates and reduces early pregnancy loss rates according to new meta analysis
This publication compares available randomised control trials (RCTs) on time-lapse versus traditional embryo incubation and evaluation to assess the effect of time-lapse and concludes that using time-lapse as a complete system helps to improve clinical outcome rates.
Key findings
Time-lapse is defined as an intervention that comprises undisturbed culture and the use of the information provided by time-lapse for embryo evaluation. Thorough analysis of available literature supports the use of time-lapse in a clinical setting: Application of time-lapse significantly improves ongoing pregnancy and live birth rates compared to traditional culture and evaluation Application of time-lapse significantly reduces early pregnancy loss rates
Objective
To assess and quantify the potential effect of applying time-lapse as a complete system for culture and selection of embryos in clinical IVF using correct methodology.
Methods
Meta-analysis of literature identified as eligible to the criteria (Randomised Controlled Trials prospectively allocating patients to time-lapse vs traditional culture and/or evaluation).
Results
Five prospective randomised controlled trials met the criteria for inclusion. All of those used either Primo Vision or EmbryoScope time-lapse systems and comprised a total of 1637 patients randomised to time-lapse or traditional culture and evaluation.
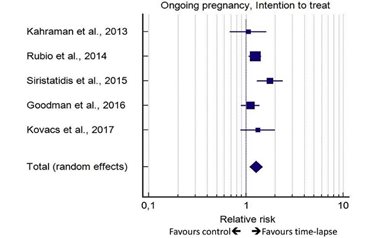
The ongoing pregnancy rate was significantly better with time-lapse (51.0%) vs. traditional methods (39.9%), p<0.001 (Odds ratio: 1.542, CI: 1.211-1.965).
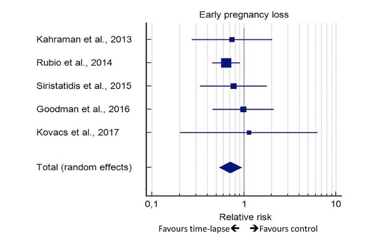
Importantly also the early pregnancy loss rate was significantly improved with the application of time-lapse and went from 21.3% with traditional methods to 15.3 with time-lapse use (Odds ratio: 1.662, CI: 0.469-0.935, p=0.019).
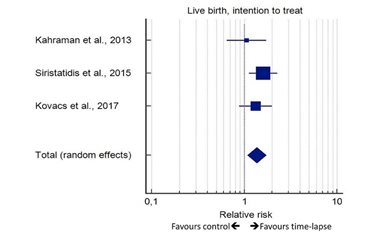
Notably, the live-birth outcome rate increased significantly with the use of time-lapse from 31.3% to 44.2% (Odds ratio: 1.668, CI: 1.134-2.455, p<0.001), however, data on live-birth rate were only available for 3 of the 5 RCTs.
The analysis showed no difference in still birth rate between the two methods.
The figures depict forest plots of the analysis of data on ongoing pregancy (figure 1a from publication, n=1637), early pregnancy loss (figure 1b from publication, n=904) and live birth (figure 1c from publication, n=481). Ongoing pregnancy and live-birth is based on intention to treat whereas the data basis for early pregnancy loss is calculated only from cases with a confirmed pregnancy.
In a forest plot, a vertical line reflects “no effect” whereas a square represents the odds ratio for each study. Square size reflects the weight of each study in the analysis and associated confidence intervals are indicated by horizontal lines. A diamond shape reflects the total effect from the meta-analysis.
In all of the below outcome analysis, data favors the time-lapse protocol defined as undisturbed culture and evaluation by inclusion of time-lapse based algorithm.
Conclusions
A thorough analysis of available eligible RCTs supports the use of time-lapse in clinical IVF by adding to the growing evidence of it’s clinical benefits.
Read the open access publication here.
Reference
Csaba Pribenszky* (University of Veterinary Science), Anna-Maria Nilselid (Vitrolife Sweden AB), Markus Montag* (ilabcomm GmbH). Time-lapse culture together with embryo selection based on morphokinetics improves pregnancy and live birth chances and reduces early pregnancy loss: a meta-analysis. Reprod BioMed Online (2017) in press: http://dx.doi.org/10.1016/j.rbmo.2017.06.022
*also work for/consult Vitrolife