Fully automated analysis
iDAScore is an AI-based scoring system that provides fully automated analysis of time-lapse sequences. Now you can get an objective ranking based on the likelihood of achieving a fetal heartbeat on days 2, 3 or blastocyst stage of each of a patient’s embryos at once – with just a touch of a button.
Learn more about iDAScore

Watch the webinar:
Embryo Evaluation's Latest Software Release: Find out what's new
Are you looking to stay up to date with the latest advancements in embryo evaluation software? Watch this short webinar, where we'll showcase the update of the iDAScore® software and its features.
Watch nowBuilding on the power of AI
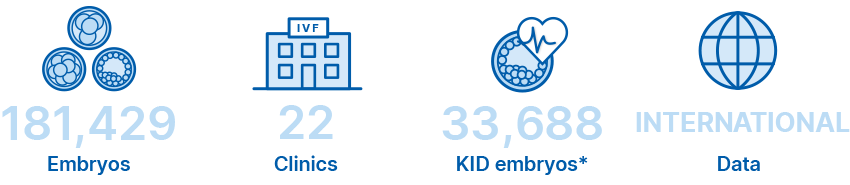
The iDAScore algorithm was developed by our own AI team and trained on full time-lapse sequences of now more than 180,000 time-lapse sequences of embryos with known clinical fate.
Diverse data to minimise bias
Data diversity and size can reduce bias in AI-based embryo selection by providing the model with a more representative sample of the population it will be used on. Diversity in the dataset means that the model is exposed to a wide variety of input patterns, which allows it to learn from a broad range of examples such as patient profile and clinical protocols. This can help to prevent the model from becoming overly specialised to a specific subset of the population, wich can lead to bias.
The iDAScore input is comprised of a wide variety of data that have been collected across three continents.The data represents a wide variety of patient profile and clinical practices including oocyte origin, IVF and ICSI, clinical protocols, and patients’ age. It includes data from both fresh and frozen embryos with known outcome.

57% more data on embryos
iDAScore has been further trained on data from an additional 65,000 embryo time-lapse sequences. iDAScore now includes embryo ranking on day 2 and day 3 in addition to blastocyst evaluation.
Performance of iDAScore
iDAScore has been validated to correlate with clinical outcomes including implantation and live birth.
Live birth rate increases by iDAScore group in all age groups3
Live Birth stratified by age of 3010 Single Vitrified Blastocyst transfers
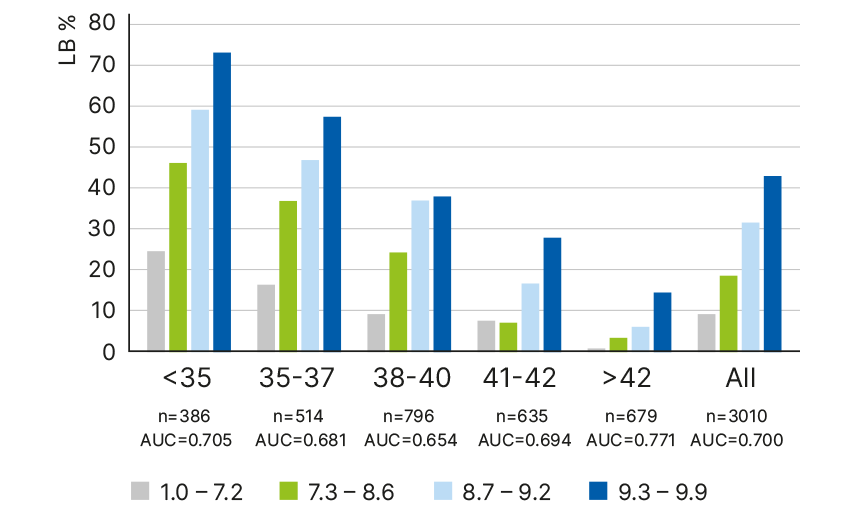
OR Live Birth 1.811 95% C.I. 1.666-1.976 p<0.05.
Multivariate adjusted OR 1.535 95%CI 1.358-1.736, p<0.05. P <0.05. for all age groups. OR = 1,811 (1.666-1.976).
aOR = 1.535 (1.358–1.736). n= # transfers in each age group.
The higher the iDAScore the higher the likelihood of implantation4
Implantation rate
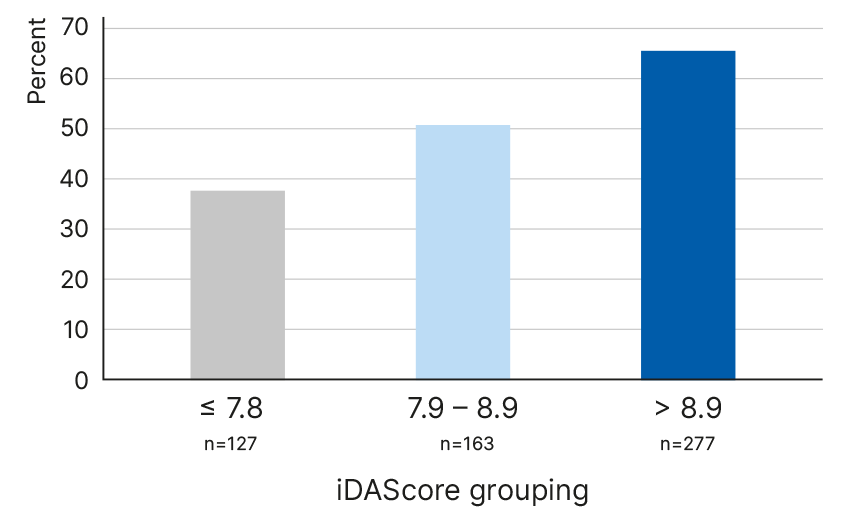
OR Oocyte donor 1.61 1.19-2.19 p<0.001
OR autologoous 1.52 1.22-1.90 p<0.001
Our findings confirm that embryo evaluation can be performed automatically allowing embryologists to utilise their time more efficiently in other tasks of the IVF process that are more complex and require high precision and attention.
Explainability AI
Rather than assigning weight to any individual event, all development events are taken into consideration in the context of the entire development sequence. Although iDAScore does not specifically use any particular parameters to generate a score, it correlates well with known features of embryo development linked to viability.
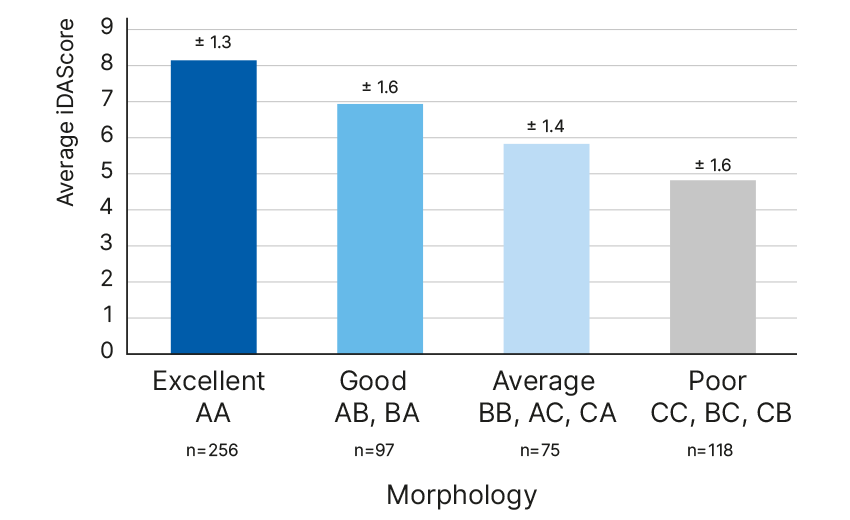
iDAScore correlation with embryologist’ gradings5
Association between iDAScore v1.0, senior embryologists’ grading
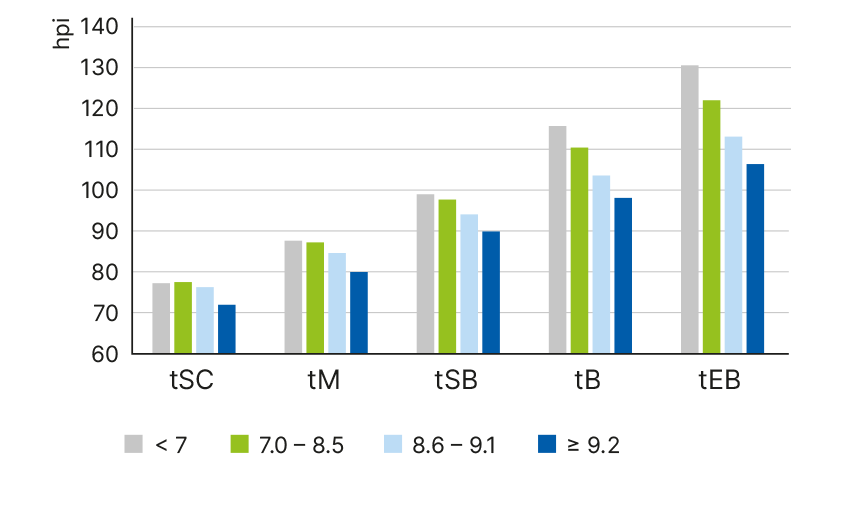
iDAScore is related to pace of development6
iDAScore group and development pace
Blastocyst with higher iDAScore have fewer cell exclusions7
Percentage blastocysts with cells excluded before compaction
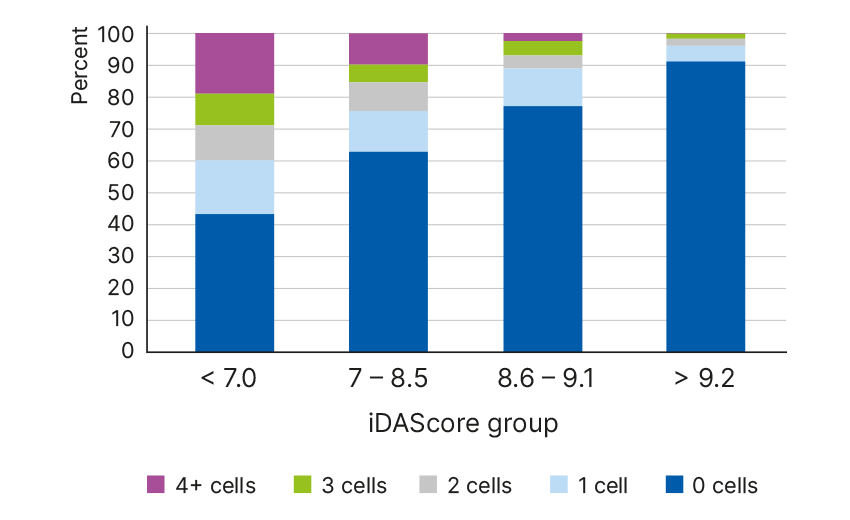
n=1503 blastocysts analysed
p<0.0001 for each morphokinetic interval
iDAScore is related to direct cleavages7
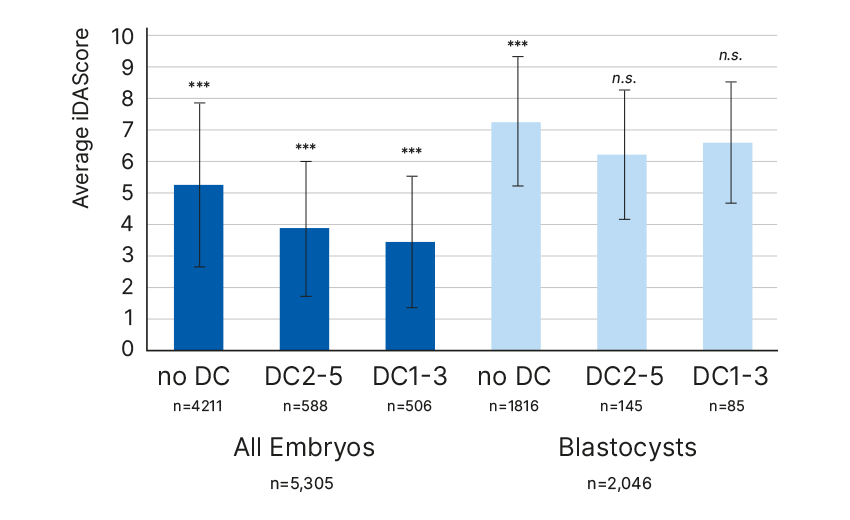
DC1-3: t3-tPNf < 5 hours, DC2-5: t5-t3 < 5 hours
“iDAScore does not require any manual, user-dependent annotations, enabling objective assessment of embryos that are cultured to the blastocyst stage. Therefore, iDAScore is an optimal method for scoring embryos and prioritising blasto- cysts for transfer without compromising live birth and neonatal outcomes.” 3
“Our findings confirm that embryo evaluation can be performed automatically allowing embryologists to utilise their time more efficiently in other tasks of the IVF process that are more complex and require high precision and attention.” 4
"With just a touch of a button, it provides us with scores instantly. It is impressive and this helps us improve our workflow and efficiency dramatically as there will be no need for annotations. It is a great tool for improving consistency in our evaluations as well.”
-Hana Watanabe, Embryologist, Hiroshima HART Clinic, Japan

“With a clear easy to use interface iDAScore makes choosing between multiple blastocysts an easier job. The score matches well with the decisions of experienced embryologists, and KIDScore D5. We think that in time, iDAScore will become an invaluable tool in helping to make our day to day clinical decisions. In addition, we are hoping to use it to assess already frozen embryos which were cultured in the EmbryoScope+. ”
-Alan Birks, Senior Clinical Embryologist
Manchester Fertility, UK

"iDAScore provides an impressive ranking of embryos. We see that the correlation with implantation, shows the same positive trend as with the KIDScore D5 decision support tool. This could be a game changer in the future of embryo evaluation, as we gain more trust in using AI for embryo evaluation.”
-Tony Price, Embryology Manager
Wessex Fertility, UK

“iDAScore is an ideal tool for providing a fast prioritization of embryos for further examination. This is especially useful for guiding new embryologists and helping them to evaluate embryos in a way that is more consistent with evaluation by senior staff with many years of experience.”
-Kirsten Simonson, Clinical embryologist
Maigaard fertility, Denmark

Explore the latest publications about iDAScore®
In this summary, we have curated the latest science publications and selected abstracts about iDAScore for your easy access. Discover articles that cover topics such as deep learning for embryo selection across multiple transfer days, validations, comparison of performances and much more.
Stay up to date - read nowA complete solution with the world’s leading time-lapse systems
Vitrolife has everything your clinic needs to maximise time-lapse culture and evaluation. Whether you want to implement and enjoy the benefits of an integrated time-lapse system for 8, 15 or 24 patients or complement your current set-up with more time-lapse incubation capacity.
Get in touch
Don't hesitate to contact us or your sales rep if you have any questions or want more information about iDAScore.
Contact usReferences
1. Bormann et. al (2020), Fertil Steril 113(4): 781-787.e1.
2. Storr et. al (2017), Hum Reprod 32(2): 307-314.
3. Ueno et al. (2022), JARG (39) 2089-2099.
4. Bori et al. (2022), Human Reproduction 37(Suppl.1).
5. Casciani et al. (2022), Human Reproduction 37(Suppl. 1).
6. Ezoe et al. (2022), Reprod Biomed Online 45(6):1124-1132.
7. Berntsen et al. (2022), PLoS ONE 17(2): e0262661.

 8 culture dish positions per incubator
8 culture dish positions per incubator

 24 culture dish positions per incubator
24 culture dish positions per incubator